Cord Blood
Saving your baby’s cord blood may be one of the best protections you can give your child
Main navigation
What is umbilical cord blood?
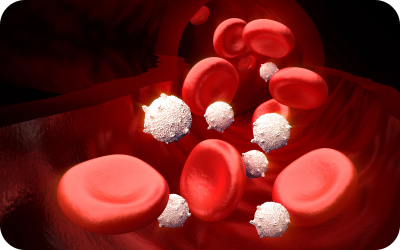
Umbilical cord blood is the blood that remains in the umbilical cord and placenta following the birth of a baby and after the umbilical cord is cut.
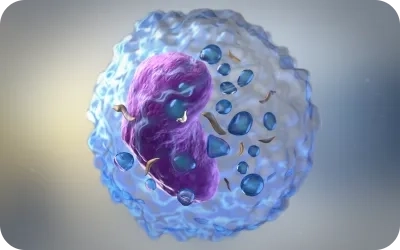
Cord blood is a rich source of hematopoietic stem cells or HSCs that have the ability to differentiate into red blood cells responsible for the oxygenation of the blood, into white blood cells which assist in antibody stimulation and fight infection, and into platelets which are involved in the clotting process.

Diseases Treated with Cord Blood Stem Cells & Other Potential Applications
Standard Therapies
Blood Cancers
- Acute Myelogenous Leukaemia
- Acute Lymphoblastic Leukaemia
- Chronic Myelogenous Leukaemia
- Histiocytic Neoplasms
- Other Myeloproliferative Neoplasms
- Myelodysplastic Syndrome
- Multiple Myeloma
- Plasma Cell Leukaemia
- Systemic Mastocytosis
- Waldenstrom Macroglobulinemia
Solid Tumors
- Hodgkin Lymphoma
- Non-Hodgkin Lymphoma
- Langerhans Cell Histiocytosis
- Neuroblastoma
- Retinoblastoma
Non-malignant Blood Disorders
- Aplastic Anemia
- Chediak-Higashi Syndrome
- Congenital Dyserythropoietic Anemia
- Diamond-Blackfan Syndrome
- DiGeorge Syndrome
- Evans Syndrome
- Fanconi Anemia
- Glanzmann Thrombasthenia
- Gunther Disease (erythropoietic porphyria)
- Hereditary BM Failure Syndromes
- Hemophagocytic Lymphohistiocytosis
- Leukocyte Adhesion Deficiency
- Paroxysmal Nocturnal Hemoglobinuria
- Pure Red Cell Aplasia
- Sickle Cell Anemia
- Thalassemia Major
Immunodeficiency Disorders
- Chronic Granulomatous Disease
- Common Variable Immunodeficiency
- Cartilage-Hair Hypoplasia
- Reticular Dysgenesis
- Severe Combined Immune Deficiency (SCID)
- Shwachman-Diamond Syndrome
- Wiskott-Aldrich Syndrome
Metabolic Disorders
- Adrenoleukodystrophy
- Gaucher Disease
- Hurler Syndrome
- Hunter Syndrome
- Krabbe Disease
- Lesch-Nyhan Syndrome
- Maroteaux-Lamy Syndrome
- Metachromatic leukodystrophy
- Osteopetrosis
- Sly Syndrome, Beta-Glucuronidase Deficiency
- Wolman Disease
Clinical Trials
- Autism
- Brain Tumor
- Cartilage Repair
- Cleft Palate Repair (Alveolar)
- Cerebral Palsy
- Crohn Disease
- Critical Limb Ischemia
- Diabetes Type 1
- Epidermolysis Bullosa
- Ewing Sarcoma
- Graft-versus-Host Disease (GvHD)
- Hypoxic Ischemic
- Encephalopathy (HIE)
- Hearing Loss
- HIV
- Ischemic Stroke
- Lupus
- Multiple Sclerosis
- Myocardial Infarction
- Ovarian Cancer
- Rheumatoid Arthritis
- Spinal cord injury
- Scleroderma
- Testicular Tumour
Quick facts about Umbilical Cord Blood Stem Cells
Youngest & most potent adult stem cells
More than 801diseases including leukemia and other blood cancers can be treated with stem cells, such as those found in the umbilical cord blood.

Individuals may need stem cell transplant in their lifetime.

Easy and Painless Collection from Umbilical Cord
Cord Blood Unit is readily available

Treatment Type
Standard treatment: blood,
immune and metabolic disorders
Potential treatment: cerebral
palsy, autism, spinal cord injury